Table of Contents
I. The Road to Liver Health: Meet Your Mighty Liver
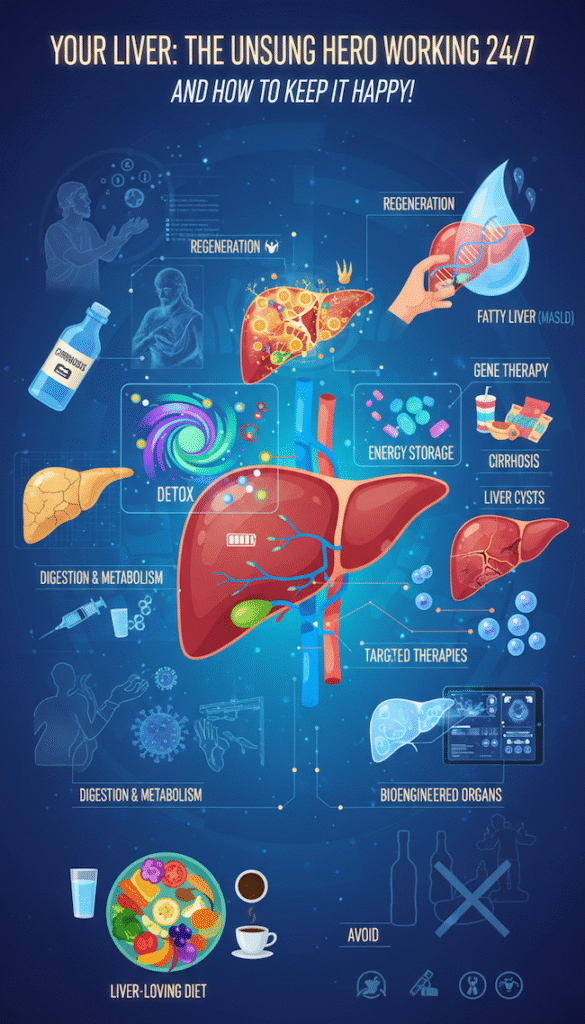
Ever think about the organ doing hundreds of vital jobs inside you quietly, efficiently, and without complaint? That’s your liver, folks.
Nestled high in the upper right of your abdomen and weighing around 3 to 5 pounds, this reddish-brown powerhouse is your body’s metabolic command center. The liver quietly handles hundreds of behind-the-scenes jobs: it filters toxins, supports digestion, processes nutrients, and tucks away vitamins and minerals for later use. And here’s the amazing part, it can actually grow back. Even after injury, it keeps repairing itself, demonstrating a remarkable resilience that offers a comforting reassurance about your health.
So why does liver health deserve more of our attention? Because this stoic workhorse rarely complains. It often masks trouble until things reach a critical stage. By the time obvious symptoms appear, serious disease may already be underway. We take our livers for granted more often than we realize. Maybe it’s time to change that. Once you see how much this quiet organ actually does, you start to understand why it deserves some care. Learning what keeps it strong can inspire simple, lasting habits that make a real difference.
II. A Trip Down Liver History: From Ancient Wisdom to Modern Science
The liver’s story stretches back through every chapter of human history. In ancient Mesopotamia, people believed it held the key to emotions and fate, reading messages from animal livers to glimpse the future. The Greeks carried that fascination into myth such as Prometheus’s endlessly renewing liver that became a symbol of human spirit and endurance.
Centuries later, medieval scholars such as Avicenna described the liver as the body’s center of balance. They believed that when the “humors,” or bodily fluids, fell out of harmony, illness would follow. This understanding of the liver’s role in maintaining metabolic balance empowers us to make informed choices about our health. Even then, early physicians noticed that what people ate could shape the liver’s health. The Renaissance brought anatomical exploration: Leonardo da Vinci sketched the liver’s complex structure, and by the 1800s, physician René Laennec coined the term cirrhosis—from the Greek kirrhos, meaning “tawny yellow”—to describe the scars on the liver.
Fast forward to the 20th century, and science finally caught up. Researchers proved alcohol could directly damage liver cells, identified the Hepatitis B and C viruses, and developed lifesaving liver transplants, a procedure where a surgical team replaces a diseased liver with a healthy one from a donor. This procedure, while complex, has a high success rate and can significantly improve the quality of life for those with severe liver disease. What was once mystical became measurable, and modern hepatology was born.
III. The Liver Lowdown: Today’s Most Common Challenges
Despite all these breakthroughs, most people remain surprisingly unaware of what affects liver health or how easily it can be compromised.
There’s still stigma around liver disease, often tied to alcohol misuse or lifestyle judgment. In reality, many liver conditions stem from metabolic dysfunction, genetics, or environmental factors. Recognizing this helps remove blame and promotes earlier diagnosis.
Let’s look at today’s most common liver concerns:
1. Fatty Liver Disease: The Silent Surge
Once known as NAFLD, it’s now called MASLD (Metabolic Dysfunction-Associated Steatotic Liver Disease). Affecting about one in three adults in Western countries, MASLD occurs when excess fat accumulates in liver cells. Its more severe form, MASH (Metabolic Dysfunction-Associated Steatohepatitis), causes inflammation and can progress to fibrosis or cirrhosis.
The main culprits: obesity, diabetes, high cholesterol, sedentary habits, and diets high in sugary drinks and refined carbs. The condition is often silent until advanced, but here’s the good news: lifestyle changes like balanced nutrition, weight loss, and regular activity can reverse early-stage fatty liver, offering hope for those who take proactive steps to improve their health.
Peer-reviewed source: Younossi, Z. M. et al. “Global epidemiology of nonalcoholic fatty liver disease—Meta-analytic assessment of prevalence, incidence, and outcomes.” Hepatology 64.1 (2016): 73–84.
2. Cirrhosis: The Scar Tissue Story
Cirrhosis is the irreversible scarring of liver tissue. Common causes include chronic alcohol use, MASLD/MASH, and viral hepatitis. Early symptoms may include fatigue or nausea; advanced stages bring jaundice, abdominal swelling (ascites), and confusion (hepatic encephalopathy). Treatment focuses on halting further damage and managing complications.
3. Liver Cysts: Mostly Harmless Bubbles
These fluid-filled sacs are often benign and discovered incidentally. Simple cysts rarely cause trouble, though large or symptomatic ones may require treatment. Many, like Grandma Betty’s routine ultrasound discovery, need nothing more than periodic checkups.
When Liver Cysts Become Painful
In some cases, liver cysts can grow large enough to cause discomfort, fullness, or pain in the upper abdomen. If a cyst becomes painful or starts to interfere with daily life, your doctor may recommend one of the following:
- Aspiration: A radiologist uses imaging guidance to insert a thin needle and drain the fluid. However, cysts often refill, so this is typically a temporary fix.
- Laparoscopic Deroofing: A minimally invasive surgery where the top (or “roof”) of the cyst is removed, allowing it to drain permanently. This procedure provides lasting relief for most patients.
- Sclerotherapy: After aspiration, a mild chemical (like alcohol) is injected to scar the cyst lining and prevent refilling.
- Treating Underlying Causes: If the cyst is related to Polycystic Liver Disease or parasitic infection (hydatid disease), specialized medical or surgical treatment is required.
- Monitoring: Imaging follow-ups ensure that cysts don’t enlarge, rupture, or cause pressure on nearby organs.
For persistent or worsening pain, always seek evaluation by a gastroenterologist or hepatologist. Self-diagnosis or internet “remedies” for cysts can delay proper care.
4. The Diabetes Liver Connection
Type 2 diabetes burdens the liver, making patients more prone to MASLD/MASH. It’s a two-way street: a struggling liver worsens insulin resistance, creating a damaging cycle. This means that managing diabetes is not only important for controlling blood sugar levels, but also for supporting liver health. Breaking that cycle with dietary improvements and glucose control dramatically supports liver health.
Breaking that cycle with dietary improvements and glucose control dramatically supports liver health.
5. Viral Hepatitis
Chronic Hepatitis B and C continue to affect millions worldwide, often causing years of inflammation that can lead to cirrhosis. In recent decades, new antivirals and vaccines have dramatically changed that story, preventing most Hepatitis B infections and curing many cases of Hepatitis C.
IV. Hot Debates and Tricky Challenges in Hepatology
As understanding grows, so do the questions. Experts continue to wrestle with ethical and clinical dilemmas such as:
The Naming Game:
Switching from NAFLD to MASLD isn’t just semantics—it reframes the disease around metabolic dysfunction rather than exclusion of alcohol use, changing both diagnosis and research approaches.
Biopsy or Beyond:
Can non-invasive tools like FibroScan and Magnetic Resonance Elastography (MRE) replace traditional biopsies? They show great promise in detecting fibrosis without pain or risk, though biopsies remain the “gold standard.”
Early Screening:
With millions unaware they have early-stage liver disease, researchers seek cost-effective screening models to catch it before it’s too late.
The “Six-Month Rule” Debate:
The long-standing “six-month rule” asks patients with alcohol-related liver disease to stay sober for half a year before they can qualify for a transplant. In recent years, doctors have started to question whether that blanket policy is fair. Some now argue that every case should be judged individually, based on a person’s commitment to recovery and medical need.
Supplements: Buyer Beware!
“Liver detox” supplements flood the market with unverified claims. Many lack scientific backing, and some even harm the liver. Always consult your doctor before taking any herbal or over-the-counter supplement. (Notably, the FDA doesn’t regulate these products like prescription drugs.)
Breaking the Stigma Barrier:
Fear of judgment keeps many silent about symptoms. Education and empathy are key to encouraging early medical care and normalizing conversations around liver health.
V. The Healthy Liver Love Language: Diet, Lifestyle, and Smart Choices
So how do you show your liver some love? With mindful eating, moderate habits, and protective daily routines.
Feast for a Happy Liver (What to Pile on Your Plate)
Rainbow Power:
Fill your plate with colorful fruits and veggies—berries, pomegranates, leafy greens, cruciferous vegetables, and beets. These antioxidant-rich foods help reduce inflammation and oxidative stress.
Whole Grains Win:
Choose fiber-packed grains like oats, quinoa, and brown rice to support metabolic balance.
Lean & Clean Proteins:
Go for fish (Omega-3 rich), skinless poultry, tofu, lentils, and beans.
Smart Fats:
Favor olive oil, avocados, nuts, and seeds over processed oils or trans fats.
Beverage Buddies:
Water reigns supreme, but moderate coffee and green tea intake may offer protective benefits—studies link both to lower risk of chronic liver disease.
Peer-reviewed source: Kennedy, O. J. et al. “Coffee consumption and health: umbrella review of meta-analyses.” BMJ 359 (2017): j5024.
No-Go Foods (What to Ditch or Limit)
- Alcohol: The single biggest threat to liver health—reduce or eliminate it entirely.
- Sugary Drinks: High-fructose beverages drive fat buildup in liver cells.
- Fried & Processed Foods: Limit trans fats and refined oils.
- Refined Grains: Cut back on white bread, pasta, and pastries.
- Salty Processed Snacks: Excess sodium contributes to water retention and high blood pressure.
- Red & Processed Meats: Enjoy occasionally, not daily.
Lifestyle Upgrades for Liver Wellness
- Hydrate Well: Water supports toxin elimination.
- Move Often: Regular exercise improves insulin sensitivity and prevents fatty buildup.
- Prioritize Restful Sleep: Deep sleep allows cellular repair and detoxification.
- Be Medication Mindful: Follow dosage guidelines and alert your doctor to all meds and supplements (especially acetaminophen, Kava, or Black Cohosh).
- Minimize Toxins: Avoid exposure to harsh chemicals and pesticides.
- Vaccinate: Protect yourself with Hepatitis A and B vaccines.
- Reduce Stress: Chronic stress impacts hormones and immune balance—both important for liver function.
VI. The Future of Liver Care: Science Meets Hope
The field of liver medicine is advancing at breathtaking speed.
Regenerative Breakthroughs:
Stem cell therapy and 3D bioprinting may soon allow growth of new liver tissue, even entire lab-engineered organs.
Targeted Therapies:
Next-generation drugs and nanoparticles aim to repair damaged cells directly—like HRX215, currently in trials for regeneration.
Gene Editing & mRNA Therapies:
Technologies such as CRISPR-Cas9 could one day correct genetic disorders or permanently disable Hepatitis B replication.
Smarter Diagnostics:
Non-invasive “liquid biopsies,” AI-assisted imaging, and microRNA blood markers will improve early detection and tracking.
Precision Medicine:
Future treatments will be tailored to each patient’s genes, lifestyle, and specific liver condition—ushering in a new era of personalized care.
Transplant Transformation:
From better organ preservation to xenotransplantation and AI-optimized matching, transplantation is becoming safer and more efficient.
VII. Wrap-Up: Love Your Liver, Live Your Best Life
Your liver is an extraordinary, resilient organ that never clocks out. It quietly performs more than 500 essential functions every single day to keep you alive and well.
Taking care of your liver doesn’t have to be complicated. A few thoughtful habits, a bit of awareness, and regular check-ins with your doctor can go a long way toward keeping it strong. And if something feels off—like unusual tiredness, yellowing of the skin, or pain near your abdomen—it’s best not to wait. Catching problems early can make all the difference.
Your liver never takes a day off—so maybe it’s time to thank it with a little care.
References:
- Younossi, Z. M. et al. “Global epidemiology of nonalcoholic fatty liver disease—Meta-analytic assessment of prevalence, incidence, and outcomes.” Hepatology 64.1 (2016): 73–84.
- Kennedy, O. J. et al. “Coffee consumption and health: umbrella review of meta-analyses.” BMJ 359 (2017): j5024.
- American Liver Foundation. “Liver Health Information.” liverfoundation.org
- Reddy, K. R. et al. “Simple and Polycystic Liver Disease: Evaluation and Management.” Clinical Gastroenterology and Hepatology 22.3 (2024): 537–546.
Liver Health Disclaimer
This article is for informational and educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding your health, medical condition, or treatment options.